Introduction: Bridging Science and Policy
Medical research and health policy may appear to be two separate worlds—one rooted in science and discovery, and the other in governance and administration. Yet, the two are deeply interconnected. Medical research is the foundation of health policy, providing the evidence and insights that shape laws, regulations, and healthcare practices worldwide. Without research, policies would be based on assumptions rather than evidence, risking inefficiency, waste, and even harm.
In today’s complex healthcare environment, medical research and analysis serve as the compass that guides policymakers toward effective solutions. From designing vaccination campaigns to tackling non-communicable diseases, research plays a pivotal role in shaping the decisions that determine the health of populations.
What is Health Policy and Why Does Research Matter?
Health policy refers to the decisions, plans, and actions undertaken to achieve specific healthcare goals within a society. It governs everything from how healthcare systems are financed and organized to how patients receive services. Effective health policy ensures that resources are used efficiently, health inequalities are reduced, and population well-being is prioritized.
Medical research matters in this context because it provides evidence-based foundations for policy-making. Instead of relying on intuition or political pressure, policymakers can turn to scientific studies, clinical trials, epidemiological data, and systematic reviews to guide decisions. Research ensures that policies are not only practical but also ethical and sustainable.
The Evolution of Evidence-Based Policy
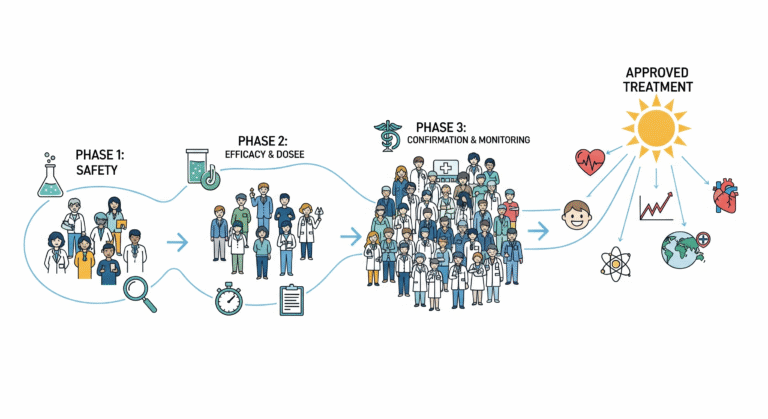
The term evidence-based policy has gained momentum in the last few decades. Inspired by the success of evidence-based medicine, it emphasizes that public health interventions and healthcare reforms should be backed by rigorous scientific evidence.
Historically, many health policies were reactive rather than proactive. For example, sanitation laws emerged in the 19th century only after outbreaks of cholera devastated communities. Over time, medical research began to highlight the causes of disease, the effectiveness of prevention, and the impact of social determinants of health. This shift allowed governments to design policies before crises occurred, rather than simply responding after the damage was done.
Today, evidence-based policy is the gold standard. It ensures that interventions are tested, analyzed, and proven effective before being widely implemented.
How Medical Research Shapes Policy Decisions
Medical research influences health policy in multiple ways. First, it identifies health priorities by uncovering the diseases and risk factors most affecting populations. For example, epidemiological studies on rising obesity rates have influenced governments to implement sugar taxes and nutritional labeling laws.
Second, research guides resource allocation. Health systems often operate with limited budgets, and medical research helps determine where investments will have the most impact. Cost-effectiveness studies, for instance, inform whether a country should prioritize expanding vaccination programs, investing in cancer treatment, or building stronger maternal health services.
Third, medical research evaluates interventions. Policies are rarely perfect from the start. By analyzing the outcomes of implemented policies, research helps refine them for greater effectiveness. Tobacco-control measures are a prime example: years of research revealed which regulations—such as taxation, advertising bans, and public smoking restrictions—work best in reducing smoking rates.
Finally, research shapes global health responses. International organizations like the World Health Organization (WHO) rely on global research data to recommend guidelines on issues ranging from pandemic preparedness to maternal health standards.
Landmark Examples of Research Shaping Policy
History provides numerous examples of how medical research has reshaped health policy:
The discovery of the link between smoking and lung cancer in the mid-20th century led to sweeping tobacco-control laws worldwide. Research into the effectiveness of vaccines transformed global health, eliminating smallpox and bringing polio to the brink of eradication. The HIV/AIDS crisis demonstrated how research on antiretroviral therapy could guide lifesaving policies, from drug accessibility programs to global awareness campaigns. More recently, during the COVID-19 pandemic, research played a critical role in shaping policies around lockdowns, mask mandates, testing, and vaccination drives.
These examples highlight a simple truth: without research, policies risk being blind guesses, but with research, they become informed strategies that save lives.
Challenges in Translating Research into Policy
While the importance of medical research is undeniable, the path from research findings to policy implementation is not always smooth. One major challenge is the time lag between discovery and policy adoption. It often takes years, or even decades, for research evidence to translate into actual reforms.
Another barrier is political influence. Sometimes, policies are shaped more by political agendas than by evidence, leading to ineffective or harmful outcomes. Misinformation also poses a major threat, as seen during the COVID-19 pandemic when conspiracy theories undermined scientifically sound policies.
Funding limitations can restrict the scope of research, while ethical challenges—such as conducting studies in vulnerable populations—can slow progress. Additionally, not all research is accessible to policymakers. Subscription-based academic journals often prevent free access, limiting the use of knowledge in low- and middle-income countries.
The Role of Medical Research and Analysis in Global Health Policy
On the global stage, medical research is essential in addressing cross-border health challenges. Pandemics, climate change, and antimicrobial resistance are not confined by geography. International collaboration in research ensures that policies are coordinated and effective.
Organizations such as the WHO, the Centers for Disease Control and Prevention (CDC), and the National Institutes of Health (NIH) depend on robust research data to issue health guidelines. For instance, CDC recommendations on vaccination schedules or WHO guidelines on nutrition are directly informed by decades of medical studies and systematic reviews