What is Public Health and Why Does It Matter?
Introduction: Health Beyond Hospitals
When people think of health, they often imagine hospitals, doctors, and medicines. But true health goes beyond individual treatment. Public health is the science and practice of protecting and improving the health of entire populations. It focuses not just on treating illness but on preventing diseases, promoting wellness, and creating healthier communities. Public health matters because it affects everyone, everywhere. From the air we breathe to the water we drink, from vaccination programs to mental health awareness campaigns, public health shapes the conditions that allow people to live healthier, longer, and more productive lives.
Defining Public Health
The World Health Organization (WHO) defines public health as “the art and science of preventing disease, prolonging life, and promoting health through the organized efforts of society.” Unlike clinical medicine, which focuses on individual patients, public health emphasizes populations. Its goal is to create conditions where people can be healthy, reducing the need for treatment in the first place. This makes public health both preventive and proactive, safeguarding communities before illness strikes.
Why Public Health Matters
Public health matters because it saves lives through prevention, reduces the financial burden of healthcare, and improves overall quality of life. Preventing disease is always more cost-effective than treating it, and public health ensures that entire populations benefit from preventive measures like vaccinations, clean water, and sanitation. It also addresses health inequalities by reaching vulnerable communities and ensures societies are better prepared for emergencies, whether pandemics, natural disasters, or environmental crises. Without robust public health systems, no amount of hospital infrastructure can prevent widespread health threats.
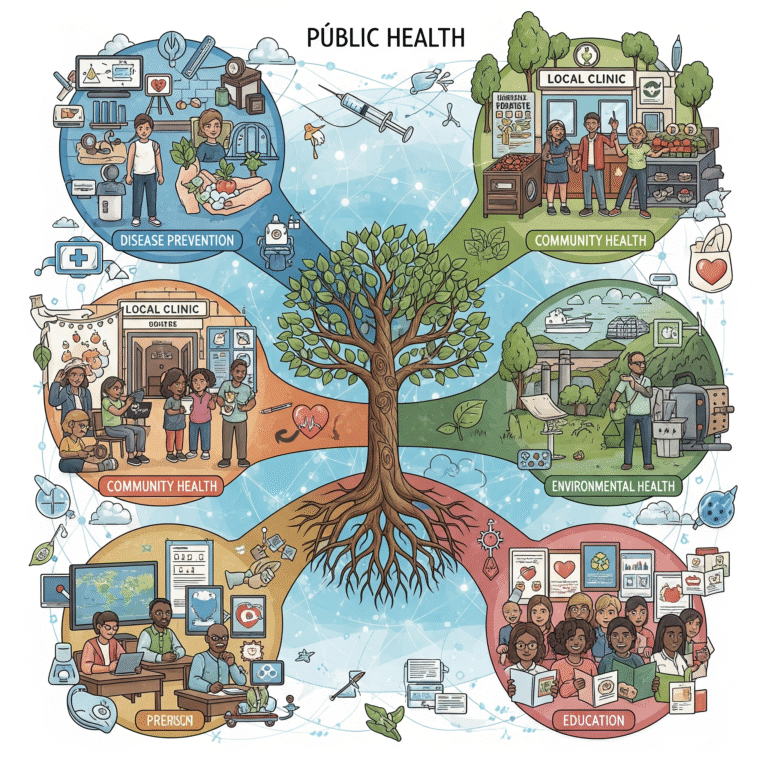
Core Functions of Public Health
Public health operates through three essential functions: assessment, policy development, and assurance. Assessment involves collecting and analyzing data about disease trends and health risks. Policy development transforms data into strategies, regulations, and interventions that guide population health. Assurance ensures that policies translate into real access to services, protecting people regardless of income or location. Together, these functions ensure that public health is evidence-based, systematic, and community-driven.
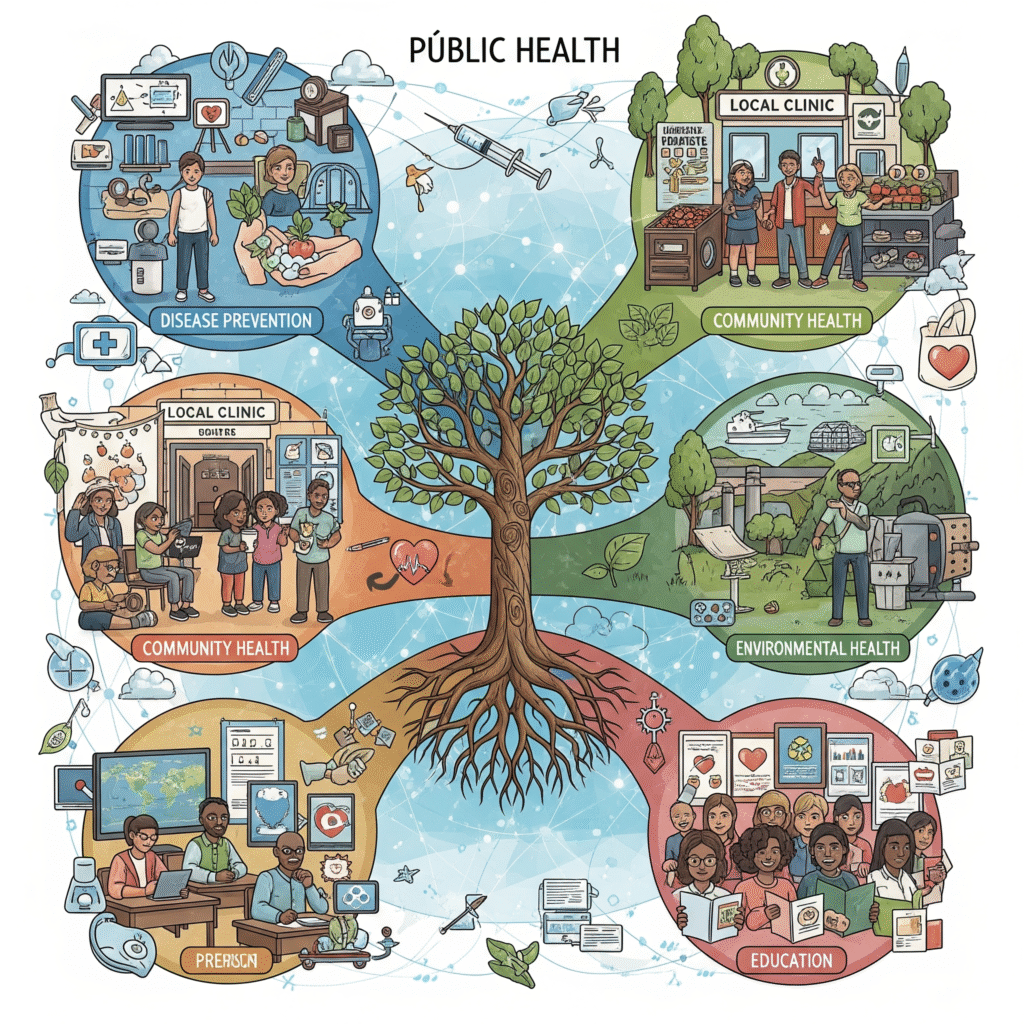
Key Areas of Public Health
Public health is a multidisciplinary field. Epidemiology studies patterns and causes of disease across populations. Environmental health ensures clean air, safe drinking water, and healthy living conditions. Health promotion encourages positive behaviors such as regular exercise, good nutrition, and mental well-being. Infectious disease control uses surveillance and vaccination to prevent outbreaks, while research on non-communicable diseases addresses conditions such as diabetes, heart disease, and cancer. Public health also focuses on maternal and child health, ensuring safer pregnancies and better outcomes for infants. On a global scale, it addresses issues that cross borders, such as climate change and pandemics, and through health policy and management, it examines how healthcare systems can be financed, organized, and delivered efficiently.
Public Health in Action
The impact of public health can be seen in real-world success stories. Vaccination campaigns have eradicated smallpox and nearly eliminated polio. Clean water and sanitation have drastically reduced waterborne illnesses such as cholera. Research linking smoking to cancer led to tobacco-control campaigns that saved millions of lives. More recently, the COVID-19 pandemic demonstrated how testing, surveillance, vaccination, and communication strategies are central to population health. Even policies such as seatbelt laws and drunk-driving restrictions emerged from public health research, saving lives on roads around the world.
Challenges in Public Health
Despite its successes, public health faces major challenges. Funding gaps often leave preventive programs under-resourced compared to hospitals and clinical treatment. Inequalities in healthcare access continue to affect disadvantaged populations. Globalization has accelerated the spread of infectious diseases, while misinformation has undermined public trust in science, particularly around vaccines. Climate change presents another critical threat, as environmental degradation, pollution, and rising temperatures introduce new health risks that require urgent attention.
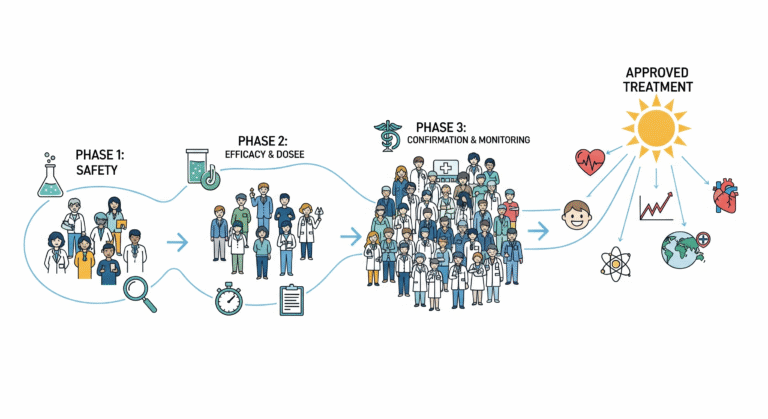
The Role of Research and Analysis in Public Health
Research and analysis are at the core of public health. Epidemiological studies allow scientists to track outbreaks, while biostatistical analysis provides clarity on large, complex datasets. Health policy research helps governments allocate resources effectively, and evidence-based medicine ensures that strategies are based on solid science rather than assumptions. Without medical research and analysis, public health would lack the knowledge base needed to prevent disease, protect populations, and evaluate the effectiveness of interventions.
Careers in Public Health
Public health also provides diverse career opportunities. Epidemiologists investigate disease outbreaks and identify their causes. Public health educators work on campaigns that raise awareness and encourage healthier lifestyles. Biostatisticians analyze research data to guide policy and practice. Policy analysts design frameworks that shape national health strategies, while environmental health experts protect communities from hazards in their surroundings. Community health workers, who often work directly with populations, play an essential role in connecting people with services and ensuring local needs are addressed.
The Future of Public Health
The future of public health will be defined by innovation and global collaboration. Digital health and artificial intelligence are transforming how diseases are monitored and prevented. Genomics and precision medicine are tailoring prevention and treatment strategies to individual risk profiles. Climate change is being recognized as a health issue, making sustainability central to future strategies. Mental health, long overlooked, is now integrated into public health planning as an essential component of well-being. Most importantly, global cooperation will be necessary to prevent and manage future pandemics, building on lessons learned from COVID-19.
Conclusion: Public Health as a Collective Responsibility
Public health is not just about preventing illness but about creating societies where people can thrive. It is the foundation of strong healthcare systems, the link between research and community, and the collective responsibility that ensures equity in health for all. By investing in public health, societies reduce healthcare costs, improve productivity, and ensure that every individual has the opportunity to live a healthier life. Its importance extends beyond medicine into social, economic, and environmental dimensions.
In the end, public health matters because it touches every aspect of human life. It ensures that vaccines reach those who need them, that water is safe to drink, that communities are prepared for health emergencies, and that preventable diseases do not overwhelm healthcare systems. Strengthening public health systems, investing in research and analysis, and promoting health equity are critical to building healthier, more resilient societies. Public health is more than a discipline; it is the backbone of progress, the safeguard of well-being, and the foundation of humanity’s collective future.